How Long Can I Live With Pavatalgia? Life Expectancy & Long-Term Outlook

Chronic pain—no matter where it begins or how it is described—affects not only a person’s physical comfort but also their emotional well-being, identity, and sense of hope. If you have recently come across the term pavatalgia, chances are you were searching for answers about a set of symptoms that have been impacting your daily life, such as persistent pain, stiffness, numbness, walking difficulty, or nerve-related discomfort. When someone types “how long can I live with pavatalgia” into a search engine, it usually reflects fear, uncertainty, and the need for clarity and reassurance.
This article takes an in-depth look at what pavatalgia represents online, whether it affects life expectancy, and how someone can live a full, meaningful life—even with chronic pain. This guide is designed in a mental-health–centric educational style to help you understand your symptoms, uncover practical tools, and regain a sense of control.
Understanding Pavatalgia: What the Internet Gets Wrong (and Why It Matters)
Before answering how long someone can live with pavatalgia, we must clarify the concept itself. Pavatalgia is not a medically recognized diagnosis in international medical classifications. Instead, the term appears mostly on blogs, symptom-explanation sites, and content platforms. Depending on the source, pavatalgia is used to describe:
- Chronic foot pain
- Knee pain resembling patellofemoral pain syndrome
- Generalized nerve pain or neuropathy
- A broader category of lower-body musculoskeletal pain
- A chronic, persistent pain pattern affecting mobility
Because these definitions vary widely, the first step in understanding your symptoms is recognizing that pavatalgia is a descriptive label, not a disease. In many cases, it acts as an umbrella term for pain caused by more specific underlying conditions such as:
- Nerve compression
- Tendon or ligament injury
- Osteoarthritis
- Peripheral neuropathy
- Overuse injuries
- Muscle imbalance
- Chronic inflammatory diseases
This distinction matters deeply. When a condition is poorly defined, people may fear the worst. When a diagnosis feels vague or unfamiliar, it creates anxiety: Is this fatal? Will it get worse? Is my life expectancy affected?
The good news is simple and reassuring:
Pavatalgia, as described on blogs and online wellness sites, is not a life-threatening condition. It does not shorten lifespan.
Instead, it affects quality of life, movement, and emotional well-being—areas you can improve with the right strategies.
Does Pavatalgia Affect Life Expectancy?
Short Answer: No—Pavatalgia Does Not Directly Shorten Your Lifespan
Whether pavatalgia is framed as foot pain, nerve pain, or knee-cap pain, available information across the internet consistently agrees:
- Pavatalgia impacts comfort, not longevity.
- People typically maintain a normal life expectancy.
- Symptoms may be chronic, but not life-shortening.
- Proper management significantly reduces long-term complications.
So if you are asking “how long can I live with pavatalgia?”, the comforting truth is:
You can live just as long as anyone else. What matters most is symptom management, not survival time.
Then why do people ask this question?
Chronic pain often creates a sense of fear, especially when it begins to affect:
- Walking ability
- Sleep quality
- Independence
- Emotional health
- Social life
People commonly interpret worsening pain as a sign of something more dangerous. Chronic pain can also lead to:
- Social withdrawal
- Depression
- Anxiety
- Reduced physical activity
All of these can influence perceived quality of life, making individuals worry about their long-term future.
However, while untreated pain can have indirect health consequences, pavatalgia as a term does not describe a fatal condition.
What Actually Influences How Well You Live With Pavatalgia?
Even though pavatalgia itself isn’t life-threatening, several factors can influence overall quality of life, mobility, and long-term well-being.
1. The underlying cause of pain
Since pavatalgia is not a formal diagnosis, the root cause determines long-term impact. Different causes come with different future expectations. Examples:
- Nerve compression → manageable with therapy, stretching, or medical treatment
- Arthritis → chronic but not deadly
- Neuropathy → depends on underlying disease
- Overuse or injury → typically improves with treatment
The more accurate your medical evaluation is, the easier it becomes to reduce symptoms and protect long-term mobility.
2. Early diagnosis and treatment
Many people live with untreated pain for years. Earlier treatment can:
- Reduce chronic inflammation
- Prevent ongoing tissue damage
- Improve mobility
- Protect mental health
- Reduce reliance on pain medications
3. Lifestyle factors
Daily habits deeply affect chronic pain. Some worsening factors include:
- A sedentary lifestyle
- Smoking
- Excess weight
- Poor posture
- Ill-fitting shoes
- Lack of stretching
- Stress and tension
Helpful lifestyle habits include:
- Gentle daily movement
- Weight management
- Strengthening exercises
- Physical therapy
- Supportive footwear
- Stretching routines
- Stress-reduction practices
4. Mental health
This is an often-overlooked piece of chronic pain. Emotional well-being affects physical discomfort through a process known as pain amplification, where stress increases sensitivity.
Common psychological challenges associated with pavatalgia include:
- Fear of movement
- Anxiety about the future
- Depression from long-term discomfort
- Social isolation
Mental health support—therapy, mindfulness, connection, coping strategies—can dramatically improve long-term outcomes.
5. Social support and lifestyle structure
People who have:
- supportive relationships
- good medical guidance
- meaningful routines
- purposeful daily activities
tend to manage chronic pain more successfully.
You won’t just “live longer”—you’ll live better.
A Deep-Dive Guide: Living With Pavatalgia Day by Day
This supportive approach prioritizes understanding, empowerment, and actionable steps. Below is an expanded, clinically informed guide for managing pavatalgia long-term.
Emotional Impact: Why Chronic Pain Feels Like a Threat to Life
Even if pavatalgia does not shorten life, it can deeply affect how people feel about their lives.
Pain wears down:
- patience
- motivation
- concentration
- self-esteem
- relationships
When discomfort is constant, the mind begins to interpret pain as danger, even when the condition itself is not life-threatening. This psychological effect makes people anxious about the future, which is often why the question “How long can I live?” surfaces.
The Mind–Pain Connection
The brain and body work together. When chronic pain persists:
- the nervous system becomes more sensitive
- stress hormones increase
- muscle tension worsens pain
- sleep quality decreases
- emotional resilience weakens
Understanding these patterns is the first step toward breaking them.
Symptoms Of Pavatalgia: A Closer Look
Even though definitions vary online, symptoms generally fall into these categories:
- Persistent foot or lower-leg pain
- Knee pain (especially around or behind the kneecap)
- Nerve-like sensations (tingling, burning, numbness)
- Stiffness after resting
- Swelling or tenderness
- Difficulty walking long distances
- Reduced flexibility or range of motion
- Pain during stairs, squatting, or standing for long periods
These symptoms affect mobility, which can influence daily life but are not associated with shortened lifespan.
How Long Can You Live With Pavatalgia? The Complete Explanation
A more complete, compassionate, and mental-health–oriented answer looks like this:
You can live a completely normal lifespan with pavatalgia. What changes is the level of comfort, not the number of years.
Your life expectancy is not reduced. However, your life satisfaction may be impacted by:
- Chronic pain
- Loss of mobility
- Emotional fatigue
- Social isolation
None of these are fatal, but all are manageable.
Key takeaway:
Pavatalgia is a long-term condition you live with, not one you die from.
Improving Quality of Life: Evidence-Informed Strategies
Below are mental-health–aligned, holistic, and medically supported methods to improve long-term life with pavatalgia.
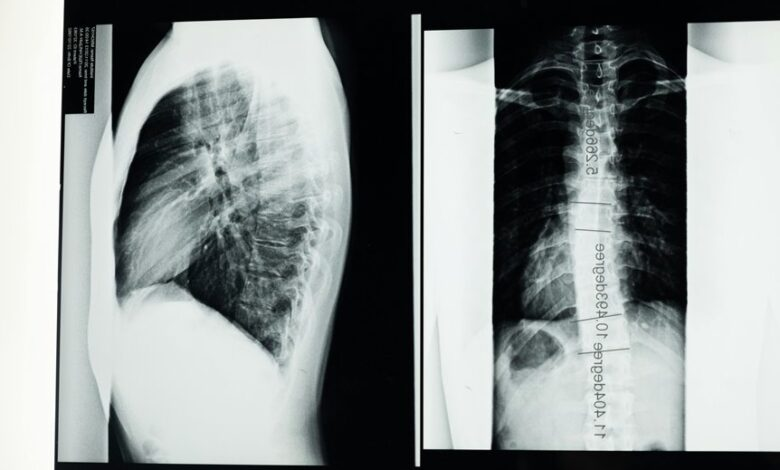
1. Medical Evaluation and Proper Diagnosis
Because pavatalgia is vague, the first step is understanding the root cause. A medical provider may recommend:
- X-rays
- MRI
- Nerve conduction studies
- Blood tests
- Mobility assessments
Accurate diagnosis dramatically improves treatment success.
2. Pain Management Strategies
For chronic pain, a multi-strategy approach works best:
- Physical therapy
- Anti-inflammatory medications
- Heat and cold therapy
- Orthotics or supportive shoes
- Stretching and strengthening
- Low-impact exercises (swimming, yoga, cycling)
- Massage therapy
- TENS units
- Posture training
Pain should be treated early—not endured.
3. Movement and Exercise
Contrary to instinct, resting too much worsens chronic pain.
Gentle movement:
- increases blood flow
- reduces inflammation
- strengthens supporting muscles
- improves mobility
- boosts mental clarity
- reduces pain sensitivity
Recommended low-impact activities:
- Swimming
- Walking with breaks
- Yoga
- Pilates
- Cycling
- Tai Chi
4. Mental Health Support
Psychological tools significantly reduce pain intensity:
- Cognitive Behavioral Therapy (CBT)
- Mindfulness practices
- Guided breathing techniques
- Pain-focused therapy
- Journaling
- Acceptance and Commitment Therapy (ACT)
These are not substitutes for medical care—they strengthen your long-term resilience.
5. Nutrition and Lifestyle
A nourishing lifestyle influences long-term comfort:
- Anti-inflammatory diet
- Hydration
- Adequate sleep
- Limiting alcohol
- Avoiding smoking
- Stress management routines
Healthy living does not cure pavatalgia, but it reduces flare-ups and improves mental health.
6. Building a Supportive Environment
Chronic pain can feel isolating. Support makes a difference:
- Family involvement
- Social connection
- Online communities
- Pain support groups
- Professional guidance
- Adaptive tools or footwear
The stronger your support system, the better your long-term outlook.
A Mental Shift: From “How Long Can I Live?” to “How Well Can I Live?”
Life with pavatalgia requires a mindset shift:
- From fear → to understanding
- From hopelessness → to strategy
- From isolation → to connection
- From vague labels → to specific treatment
- From mere survival → to meaningful living
You deserve to know that pavatalgia does not define your lifespan, your identity, or your future. What matters is building a life where symptoms are managed, your mind is supported, and you maintain your sense of purpose.
Final Thoughts: Your Life Expectancy With Pavatalgia Is Normal
Pain may change your daily experience, but it does not dictate your long-term survival. You can live a long, fulfilling life with pavatalgia when supported by a combination of:
- proper diagnosis
- physical treatment
- mental health care
- lifestyle adjustments
- supportive relationships
The goal is not only to live long, but to live well.
This detailed guide is published for readers of Newsta, supporting those who are navigating chronic pain, searching for clarity, and seeking hope for a better tomorrowFAQs — How Long Can I Live With Pavatalgia?
1. Is pavatalgia a real medical condition?
Pavatalgia is not a formally recognized medical diagnosis in standard medical systems. The term appears mostly on blogs and wellness sites to describe chronic pain in the feet, knees, or lower body. Your doctor may diagnose the real underlying cause, such as neuropathy, arthritis, or overuse injuries.
2. Does pavatalgia affect life expectancy?
No. Pavatalgia does not shorten your lifespan. It affects comfort, not survival. Most people can live a normal life expectancy with proper treatment and symptom management.
3. Why does pavatalgia feel so severe if it isn’t life-threatening?
Chronic pain affects both the body and the mind. Persistent discomfort can increase anxiety, limit mobility, and impact mood, making the condition feel more dangerous than it actually is. The emotional burden often magnifies the experience of pain.
4. Can pavatalgia get worse over time?
Yes, if left untreated. The underlying causes—such as nerve compression, arthritis, or muscle imbalance—may progress. Early diagnosis, physical therapy, and lifestyle care can prevent worsening symptoms.
5. What symptoms are commonly linked to pavatalgia?
People often report:
- Foot or knee pain
- Tingling or burning sensations
- Swelling or stiffness
- Numbness or nerve-like discomfort
- Difficulty walking or climbing stairs
- Pain after long periods of standing or rest
6. How is pavatalgia diagnosed?
Since pavatalgia itself is not a clinical diagnosis, healthcare professionals will assess the root cause. They may use imaging tests, nerve studies, mobility assessments, or blood work to identify the real condition behind your pain.
7. What treatments help relieve pavatalgia?
A combination of approaches works best:
- Physical therapy
- Pain-relief medications
- Stretching and strengthening exercises
- Orthotic footwear
- Heat/ice therapy
- Anti-inflammatory routines
- Mindfulness and stress management
- Lifestyle adjustments like weight control and improved posture
8. Can exercise make pavatalgia worse?
High-impact activities may aggravate symptoms. However, gentle movement—such as swimming, yoga, cycling, and walking—usually reduces inflammation and helps long-term pain management. A physiotherapist can recommend safe exercises.
9. Does mental health affect pavatalgia?
Absolutely. Stress, anxiety, and depression can intensify the perception of pain. Mind–body approaches like CBT, meditation, deep breathing, and counseling can significantly improve daily functioning and lessen pain sensitivity.
10. Should I worry about long-term disability?
Most people with pavatalgia do not become disabled. However, mobility issues may occur if symptoms are ignored. With early treatment, structured exercises, and consistent care, most individuals maintain normal daily functioning.
11. When should I see a doctor?
Seek medical attention if you experience:
- Persistent pain lasting longer than 2–3 weeks
- Sudden numbness or loss of strength
- Trouble walking
- Pain that interrupts sleep
- Signs of infection or inflammation
- Worsening symptoms despite home care
12. Can pavatalgia be cured?
Cure depends on the underlying cause. Some cases improve completely (e.g., overuse injuries), while others require long-term management (e.g., arthritis or neuropathy). With proper care, many people significantly reduce symptoms and regain normal mobility.
13. How can I live better with pavatalgia?
Focus on a whole-person approach:
- Treat the root medical cause
- Move gently every day
- Strengthen supporting muscles
- Prioritize mental well-being
- Build social support
- Maintain healthy lifestyle routines
- Follow a personalized treatment plan
14. What’s the long-term outlook?
Very positive. Pavatalgia does not shorten life expectancy. With consistent care, most people live long, fulfilling lives while managing symptoms effectively.